In
2012, I graduated from the University of Windsor and began my studies at the
Canadian Memorial Chiropractic College. As I now prepare to walk across the
stage this summer, my family and friends still ask me “how is physio school
going?” “Can you massage my feet for me?” “It took you eight years to become a
chiro?!” At first, it broke my heart to hear that so many people (especially my
friends and family) we ignorant to chiropractic. On top of that, it has been astonishing
to hear such questions as “are chiropractic adjustments dangerous?” or, “is it
true that chiropractic adjustments of the neck can cause stroke?” Before I go
any further, lets clear this up.
The
risk of suffering a stroke after a neck adjustment is reported to be less than
1 in 3 million. To put this into perspective, the odds of being struck by
lightning in Canada are 1 in about 960,000. You’re greater than three times
more likely to be struck by lightening than suffer a stroke after a visit to
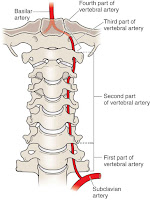
your chiropractor! The theory is that an adjustment of the neck may cause a dissection
of the vertebral artery. Dissection (or tearing) of this artery may compromise
blood flow to the brain, causing stroke. Research has show that more stress is
placed on the vertebral artery when you check you’re blind spot while driving.
Would you refrain from checking you’re blind spot while driving in fear of
suffering a stroke? I guess that’s up to you.
Right Vertebral Artery
The
stroke statistic is only based on a temporal relationship; patients who
suffered a stroke reported receiving spinal manipulation as far as 2 weeks
before the stroke was detected. This is a typical case of being at the wrong
place at the wrong time. To date, there have been no studies showing that
spinal manipulations (ie. adjustments) CAUSE a stroke. Statistics show that you
are more likely to suffer a stroke after visiting your medical doctor! Once
again, this is a temporal relationship.
During the initial stages of a stroke, symptoms may mimic
musculoskeletal problems, such as neck pain, headaches, dizziness, blurry
vision and so on. When these patients visit their health care professionals, or
in this case their chiropractors, a stroke may already be in progress, but they
are not aware of it. If a proper and
through examination of the patient is not completed, a stroke may go undetected
until the condition has progressed significantly, after a visit with their
health practitioner. Similar statistics are seen with low back adjustments and
disc herniation.
Let’s
get back on track now. What is Chiropractic? As described by the Ontario
Chiropractic Association (OCA):
“Chiropractic is one of the largest primary health
care professions in Ontario. It is a non-invasive, hands-on health care
discipline that focuses on the musculoskeletal system. Chiropractors practice with
a manual approach, providing diagnosis, treatment and preventive care for
disorders related to the spine, pelvis, nervous system and joints. Chiropractors
use a combination of treatments, all of which are predicated on the specific
needs of the patients. After taking a complete history and diagnosing a
patient, a chiropractor can help develop and carry out a comprehensive
treatment/management plan, recommend therapeutic exercise and other non-invasive
therapies, and provide nutritional, dietary and lifestyle counselling.”
Chiropractors
manage physical conditions involving the nervous system and musculoskeletal
system. A common question I hear is “what is the difference between a
chiropractor and a physiotherapist?” There are many similarities in the scopes
of practice of these two health professions. The main thing that I believe sets
us apart from other manual therapists is our expertise in administering spinal
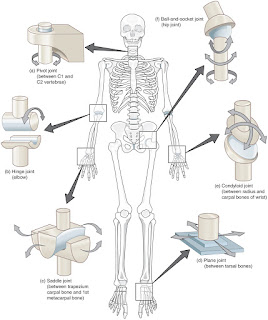
manipulative therapy (SMT), aka “the adjustment”. SMT can be described as taking a joint to its passive end-range, then
applying a high-velocity low-amplitude thrust to take that joint to its
paraphysiological space. This space is found just past the passive
end-range of a joint, without causing tissue damage. When this space is reached
with SMT, an audible “pop” or “crack” can be heard, which is termed a “cavitation”. There is some controversy with
the cause of the cavitation. Previous
theories suggested the cavitation to be the popping of gaseous bubbles. Most
recent research has used MRI for real-time visualization of joint cavitation in
knuckles. This study has shown joint cavitation to be due to tribonucleation: the rapid separation
of surfaces (in this instance the articulating surfaces of two bones) with
subsequent cavity (space) formation (Kawchuk, et al. 2015). If you are
interested in seeing what cracking you’re knuckles looks like with MRI, check
out the YouTube link below:
SMT
can be applied to any synovial joint in the body. A synovial joint is when two
bones meet and are connected by a fibrous joint capsule. Within this capsule,
the joint cavity is filled with synovial fluid, which acts to reduce friction
between the articulating bone surfaces. For numerous reasons, a joint can
become restricted. Inadequate movement and reduced joint space can lead to
degeneration of the cartilage and pain of the joint. This is commonly referred
to as “arthritis” (joint inflammation) or “arthralgia” (joint pain). SMT can be
used in both acute and chronic joint issues to improve joint function and joint
health. Aside from its local effects on the joint, SMT has also been shown to
act as an analgesic, improve neurological function, improve muscle function and
influence hormonal levels. When a joint is moved within its passive-end range,
it is referred to as a joint “mobilization”.
As
chiropractors, SMT is our bread and butter. It is what sets us apart from other
manual therapy disciplines. Students at CMCC participate in over 4,200 hours of
academic and clinical education, which is comparable to, if not more than, most
medical doctor programs. In the first three years, 336 hours are devoted to the
hand-on practice of assessments and treatments, including the SMT. The 4th
year involves a 12-month internship of providing chiropractic care under the
license and supervision of an experience chiropractor. This internship includes
1000 hours of working in a clinic with a minimum of 250 SMT’s provided during a
minimum of 380 patient treatments. No other health profession receives this
much training and practice in the application of SMT.
Although
joint manipulation can be applied to many joints in the body, there are 3
particular cases that I wanted to highlight: low back pain, neck pain and
headaches.
Low
back pain
(LBP) is very common. Up to 84% of adults have low back pain at some point in
their lives, and greater than 25% report low back pain in the last 3 months. In
the US, health care expenditure for low back pain in 1998 was estimated at $90
billion. Since then, costs of low back care have risen. Low back pain is one of
the most common reasons for missed work or reduced productivity while at work,
resulting in high indirect costs. LBP can
be classified as acute (lasting <6 weeks), subacute (lasting 6-12 weeks) and
chronic (lasting >12 weeks). Some key studies on low back pain and spinal
manipulation (AHRQ, 2016) are highlighted below.
· Acute LBP
o
2
trials found SMT to be associated with better effects on function versus sham
SMT. Effects on pain favoured manipulation, but this finding was not
statistically significant.
o
1
trial found patients with acute or subacute LBP found SMT associated with
moderate effects vs. usual care on pain and small effect on function at
short-term follow-up.
o
4
trials found SMT plus either exercise or advice associated with greater
improvement in function at 1 week versus exercise or advice alone (no
difference at 1 month or 3 months).
· Chronic LBP
o
1
high quality trial found SMT associated with greater improvement in the “main
complaint” vs. an inert treatment.
o
A
systematic review found SMT associated with better short-term relief vs. other
active interventions at 1 month and 6 months. SMT was also associated with greater
improvement in function versus other active interventions at 1 month.
o
A
systematic review found spinal manipulation plus another active treatment
associated with greater pain relief at 1 month, 3 months and 12 months versus
other treatment alone. This combination therapy was also associated with better
function at 1 month, 3 months and 12 months.
· Radicular low back pain
(example, sciatica)
o
1
good-quality trial found SMT plus home exercise and advice associated with
greater improvement in leg and back pain in 12 weeks versus home exercise and
advice alone.
· No serious adverse
events were reported and most adverse events were related to muscle soreness or
transient increase in pain.
Neck
Pain,
as described by the Ontario chiropractic association (OCA), can be broken down
into non-specific (not due to whiplash) and whiplash-associated.
· Non-specific à The annual prevalence of non-specific
neck pain (aka “mechanical neck pain”) is estimated to range between 30-50%.
Persistent or recurrent neck pain is reported by 50-85% of patients 1-5 years
after initial onset. Its course is usually episodic and complete recovery is
uncommon for most patients. 27% of patients seeking chiropractic treatment
report neck problems.
o
Acute
§ SMT is recommended for
the treatment of acute neck pain for both short- and long-term benefit (days to
recovery, pain) when used in combination with other treatment modalities
(advice, exercise, and mobilization).
§ Mobilization is
recommended for the treatment of acute neck pain for short-term (up to 12
weeks) and long-term benefit (days to recovery, pain) in combination with
advice and exercise.
§ Home exercise with
advice or training is recommended in the treatment of acute neck pain for both
short and long-term benefits (neck pain)
o
Chronic
§ SMT is recommended in
the treatment of chronic neck pain for short and long-term benefit (pain, disability)
§ SMT is recommended in
the treatment of chronic neck pain as part of a multimodal approach for both
short- and long-term benefit (pain, disability, neck range of motion).
§ Mobilization is
recommended for the treatment of chronic neck pain for short-term (immediate)
benefit (pain, neck range of motion)
§ Manual therapy is
recommended in the treatment of chronic neck pain for the short and long-term
benefit (pain, disability, neck range of motion, strength) in combination with
advice, stretching and exercise.
· Whiplash-associated
disorders
(WAD) à WAD of the neck is
further divided into 4 categories (WAD 1 to 4). 90% of WAD cases are diagnosed
as type 2 – a whiplash injury with neck symptoms (pain and stiffness),
musculoskeletal signs and substantial interference with activities of daily
living (ex. Point tenderness, decreased neck range of motion). Recommendations
for SMT vary, depending on the time frame since injury.
o
Very
low-frequency of SMT is recommended in the initial 7 days post-injury
o
High
frequency of SMT is recommended from 1 to 12 weeks post-injury
o
Low
to medium frequency of SMT is recommended greater than 12 weeks post-injury.
Headaches, based on patient
history and physical examination, can be further classified into 3 types:
migraine, tension-type and cervicogenic.
· Migraine
o
SMT
is recommended for the management of episodic or chronic migraine (with or
without aura)
o
Multimodal
multidisciplinary care (exercise, relaxation, stress and nutritional
counseling, massage therapy) is recommended for the management of episodic or
chronic migraine
· Tension type
o
Low-load
craniocervical mobilization is recommended for longer term (ex. 6 months)
management of patients with episodic or chronic tension-type headaches
o
SMT
cannot be recommended for episodic tension-type headaches, and a recommendation
cannot be made for or against the use of SMT for chronic tension-type
headaches.
· Cervicogenic
o
SMT
is recommended for the management of cervicogenic headache.
o
Joint
mobilization is recommended for cervicogenic headache.
o
Deep
neck flexor exercises are recommended for cervicogenic headache.
Low
back pain, neck pain and headaches are the most common conditions treated by
chiropractors. However, there is much more chiropractors can help with,
including, but not limited to:
· Strains and Sprains
· Repetitive strain
injuries
· Work and sports injuries
· Arthritis
· Limited range of motion
in joints
· General health and
well-being
For
more information on what a chiropractor can do for you, you can visit the
Ontario Chiropractic Association website, ask your Catalyst chiropractor or ask
myself. Stay active and stay healthy!
Mitch Broser
Strength & Conditioning Specialist
Resources:
1.
Cassidy
JD, et al. risk of vertebrobasilar stroke and chiropractic care. Spine. 2008.
33:4S; S176-S183.
2.
Kawchuk
GN, Fryer J, Jaremko JL, Zeng H, Rowe L, Thompson R (2015) Real-Time
Visualization of Joint Cavitation. PLoS ONE 10(4): e0119470.
doi:10.1371/journal.pone.0119470
3.
Effective
health care program. Noninvasive treatments for low back pain. Comparative
effectiveness review, number 169. Agency for healthcare research and quality,
2016.
4.
Clinical
practice guideline for the chiropractic treatment of adults with neck pain.
2014. (available at: www.chiropracticcanada.ca)
5.
Practice
guide for the management of whiplash-associated disorders in adults. 2010.
(available at www.ccachiro.org).













0 comments:
Note: only a member of this blog may post a comment.